
Boosting activity in brain areas related to thinking and problem-solving may also buffer against worsening anxiety, suggests a new study by Duke University researchers.
Using non-invasive brain imaging, the researchers found that people at-risk for anxiety were less likely to develop the disorder if they had higher activity in a region of the brain responsible for complex mental operations. The results may be a step towards tailoring psychological therapies to the specific brain functioning of individual patients.
“These findings help reinforce a strategy whereby individuals may be able to improve their emotional functioning -- their mood, their anxiety, their experience of depression -- not only by directly addressing those phenomena, but also by indirectly improving their general cognitive functioning,” said Ahmad Hariri, a professor of psychology and neuroscience at Duke. The results are published Nov. 17 in the journal Cerebral Cortex.
Previous findings from Hariri’s group show that people whose brains exhibit a high response to threat and a low response to reward are more at risk of developing symptoms of anxiety and depression over time.
In the current work, Hariri and Matthew Scult, a clinical psychology graduate student in the department of psychology and neuroscience at Duke, wanted to investigate whether higher activity in a region of the brain called the dorsolateral prefrontal cortex could help shield these at-risk individuals from future mental illness.
“We wanted to address an area of understanding mental illness that has been neglected, and that is the flip side of risk,” Hariri said. “We are looking for variables that actually confer resiliency and protect individuals from developing problems.”
The dorsolateral prefrontal cortex is our brain’s “executive control” center, helping us focus our attention and plan complex actions. It also plays a role in emotion regulation, and well-established types of psychotherapy, including cognitive behavioral therapy, engage this region of the brain by equipping patients with strategies to reframe or re-evaluate their emotions.
The team drew on data from 120 undergraduate students who participated in the Duke Neurogenetics Study. Each participant completed a series of mental health questionnaires and underwent a type of non-invasive brain scan called functional Magnetic Resonance Imaging (fMRI) while engaged in tasks meant to activate specific regions of the brain.
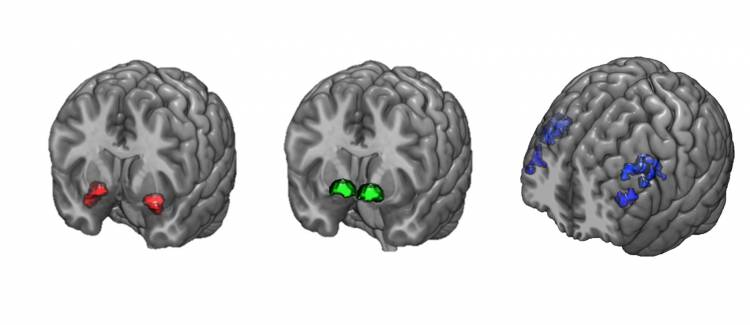
The researchers asked each participant to answer simple memory-based math problems to stimulate the dorsolateral prefrontal cortex. Participants also viewed angry or scared faces to activate a region of the brain called the amygdala, and played a reward-based guessing game to stimulate activity in the brain’s ventral striatum.
Scult was particularly interested in “at-risk” individuals with the combination of high threat-related activity in the amygdala and low reward-related activity in the ventral striatum. By comparing participants’ mental health assessments at the time of the brain scans, and in a follow-up occurring on average seven months later, he found that these at-risk individuals were less likely to develop anxiety if they also had high activity in the dorsolateral prefrontal cortex.
“We found that if you have a higher functioning dorsolateral prefrontal cortex, the imbalance in these deeper brain structures is not expressed as changes in mood or anxiety,” Hariri said.
The dorsolateral prefrontal cortex is especially skilled at adapting to new situations, the researchers say. Individuals whose brains exhibit the at-risk signatures may be more likely to benefit from strategies that boost the brain’s dorsolateral prefrontal activity, including cognitive behavioral therapy, working memory training, or transcranial magnetic stimulation (TMS).
But, the researchers warn, the jury is still out on whether many brain-training exercises improve the overall functioning of the dorsolateral prefrontal cortex, or only hone its ability to complete the specific task being trained. Additional studies on more diverse populations are also needed to confirm their findings.
“We are hoping to help improve current mental health treatments by first predicting who is most at-risk so that we can intervene earlier, and second, by using these types of approaches to determine who might benefit from a given therapy,” Scult said.
The Duke Neurogenetics Study was supported by National Institutes of Health grant R01DA033369 and Duke University. Additional support for this research was provided by National Institutes of Health grant R01AG049789 and a National Science Foundation Graduate Research Fellowship.
CITATION: "Prefrontal Executive Control Rescues Risk for Anxiety Associated with High Threat and Low Reward Brain Function," Matthew A. Scult, Annchen R. Knodt, Spenser R. Radtke, Bartholomew D. Brigidi and Ahmad R. Hariri. Cerebral Cortex, Nov. 17, 2017 (online) DOI: 10.1093/cercor/bhx304