With a crackle, a hiss and a low background hum, the sounds of one mouse thinking are coming in at the rate of one data point every 1.6 milliseconds for each of 96 individual neurons firing information along the brain's neural networks. In the lab of Kafui 'Kaf' Dzirasa, PhD'07, MD'09, neurobiologists are listening in as the mouse explores its environment, eats, grooms itself and interacts with other mice.
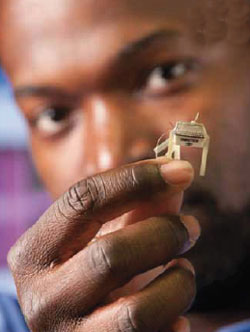
Individual electrodes in a paper-thin microarray half the size of a postage stamp record the brain's electrical patterns in real time, allowing the researchers to follow complex patterns of behavior for the first time. The project's goal is no less than to map the abnormal patterns responsible for mental illnesses, with an eye toward developing new forms of therapy targeted to correcting specific patterns of brain activity.
"Our framework for thinking about mental illnesses has to change," he says. "This is what drives me: addressing these illnesses."
Combining the cool reasoning of an engineer and the compassion of a doctor seeking help for his patients, Dzirasa wants to unite the fields of neurobiology and psychiatry behind a new understanding of psychiatric illness based on patterns of neural networks, not subjective evaluations of symptoms.
"These illnesses still carry a stigma," he says. "If we could show that these illnesses are simply a network problem, and we could provide a network solution, it could remove some of that stigma."
He sees the work at the Duke Institute for Brain Sciences (DIBS) as the logical next step in research that has allowed doctors to bypass damaged nerves in an amputated arm. If it's possible to teach the brain to manipulate a prosthetic limb, why not do the same for people with psychiatric illnesses, he reasons. He likens the approach to a pacemaker, which bypasses short-circuited electrical circuitry in the heart to restore a steady heartbeat.
"If you have the ability to read brain systems and circuits in real time, you could bypass the dysfunctional circuit and send the information directly to the other side to reconnect the network," he says.
The problem is that until very recently, the ability to record neural activity in the brain has been limited by a lack of tools capable of measurement in real time.
"These are ultimately network problems and we didn't have network tools until 20 years ago," says Dzirasa. Now he says, we have a framework and computing infrastructure to tackle network problems.
When Dzirasa graduated from the University of Maryland, Baltimore County, with a degree in engineering, his goal was to ask questions of the human body through the lens of engineering. He saw the human body as a complex machine, with the brain as the ultimate neural network. As an MD/PhD student at Duke, he was drawn to the work of Miguel Nicolelis, who had pioneered the use of miniature electrical circuits to measure the activity of many individual neurons firing in the brain.
"Miguel was really one of the world leaders in this area," he says. During his graduate training, and then as a post-doctoral scientist, Dzirasa built on the work of Nicolelis and Rui Costa, PhD, another Duke postdoctoral student, to expand the study from three areas of the brain to 11. This expansion allowed the group to look at electrical impulse patterns across the entire brain at the same time.
Now Dzirasa is systematically mapping the patterns of brain activity in both normal mice and mice that carry genetic defects known to be reliable models of human mental illnesses.
The research team has recently found that they could mimic the brain patterns of obsessive-compulsive disorder (OCD) in mice. When the researchers treated a normal mouse with a medication that halved the amount of the neurotransmitter norepinephrine in the brain, it radically shifted the pattern of the brain's neural network connections. At the same time, the researchers observed that the mouse began repetitive grooming behaviors. Searching through the medical literature, they discovered that the disrupted circuits they observed have also been implicated in OCD. Since low norepinephrine is not implicated in OCD, yet the pattern of brain activity was similar, the finding suggested that brain activity can be disrupted in different ways, and yet produce similar symptoms.
Dzirasa, Nicolelis, and postdoctoral scientist Sunil Kumar, along with several collaborators recently showed that mice carrying a mutation in a gene known to predispose people to bipolar disorder had disruptions in brain patterns to and from the nucleus accumbens, a portion of the brain known as our "reward" system.
"It looks like the reward area loses its functional connection with the parts of the brain that deal with fear and anxiety," he says. "We suspect that this functional change no longer allows fear or anxiety to be moved into decision-making, which is why you see the impulsivity and grandiosity in bipolar disorder. They are just not considering that something might be dangerous."
The research team was able to show that treating the mice with lithium, a common treatment for psychiatric disorders, restored normal brain patterns in the affected mice, but had no effect on the normal mice.
More recently, Dzirasa has been collaborating with Herb Covington, PhD, also a faculty member at DIBS, to examine brain patterns of mice in socially stressful situations as a model for depression and posttraumatic stress disorder (PTSD).
"We started with this idea that if we could understand the brain not from a chemical standpoint but from a network standpoint, we could apply our understanding across different disorders," he says. "For example, depression is diagnosed by a constellation of symptoms. The problem is these constellations of symptoms don't tell us about the underlying biology of the disease."
In work that is still underway, the scientists have gained hints that depression-like behaviors in mice can be reversed by stimulating specific cells that synchronize the electrical networks in the brain. The research is like a more targeted variation of deep brain stimulation currently used to treat chronic depression. The research even suggests that some mice are more emotionally resilient and less prone to depression.
"It may mean that there are subtle differences in the brain that make some of us more prone to be vulnerable to stress," he says.
By mapping these networks, Dzirasa hopes to create targeted "network tools," to treat not only depression, a condition in which the brain's networks may temporarily get derailed or change tracks, but also schizophrenia, a condition in which patients lose network connections permanently. He hopes to one day be able to reconnect these missing neural networks using his network pacemaker.
While correcting mental illnesses with a pacemaker may seem to belong to the realm of science fiction, Dzirasa and his Duke colleagues have already shown that, at least in mice, they are on a promising track.